Bursitis On The Foot And Ankle
Do you experience pain at the back of your heel? Is the back of your heel red and swollen? And you were told that it might Achilles Tendonitis? But so far treatment for Achilles Tendonitis does not seem to be working? You might be suffering instead from Retrocalcaneal Bursitis.
Causes
As ligaments and tendons stretch and tear, blood from ruptured blood vessels becomes trapped in the local tissues. As the trapped blood clots up, it sticks the tissues together creating adhesions. Adhesions cause pain, inflammation and restricted movement because the layers of tissue that used to slide smoothly across one another now adhere and snap which interferes with normal functioning. It is essential to break up clotted blood as quickly as possible to prevent adhesions and scar tissue from forming.
Symptoms
Patients with this condition typically experience pain at the back of the ankle and heel where the Achilles tendon attaches into the heel bone. Pain is typically experienced during activities requiring strong or repetitive calf contractions (often involving end of range ankle movements) such as walking (especially uphill), going up and down stairs, running, jumping or hopping (especially whilst wearing excessively tight shoes). Often pain may be worse with rest after these activities (especially that night or the following morning). The pain associated with this condition may 'warm up' with activity in the initial stages of injury. As the condition progresses, patients may experience symptoms that increase during sport or activity, affecting performance. In severe cases, patients may walk with a limp or be unable to weight bear on the affected leg. Other symptoms may include tenderness on firmly touching the affected bursa and swelling around the Achilles region.
Diagnosis
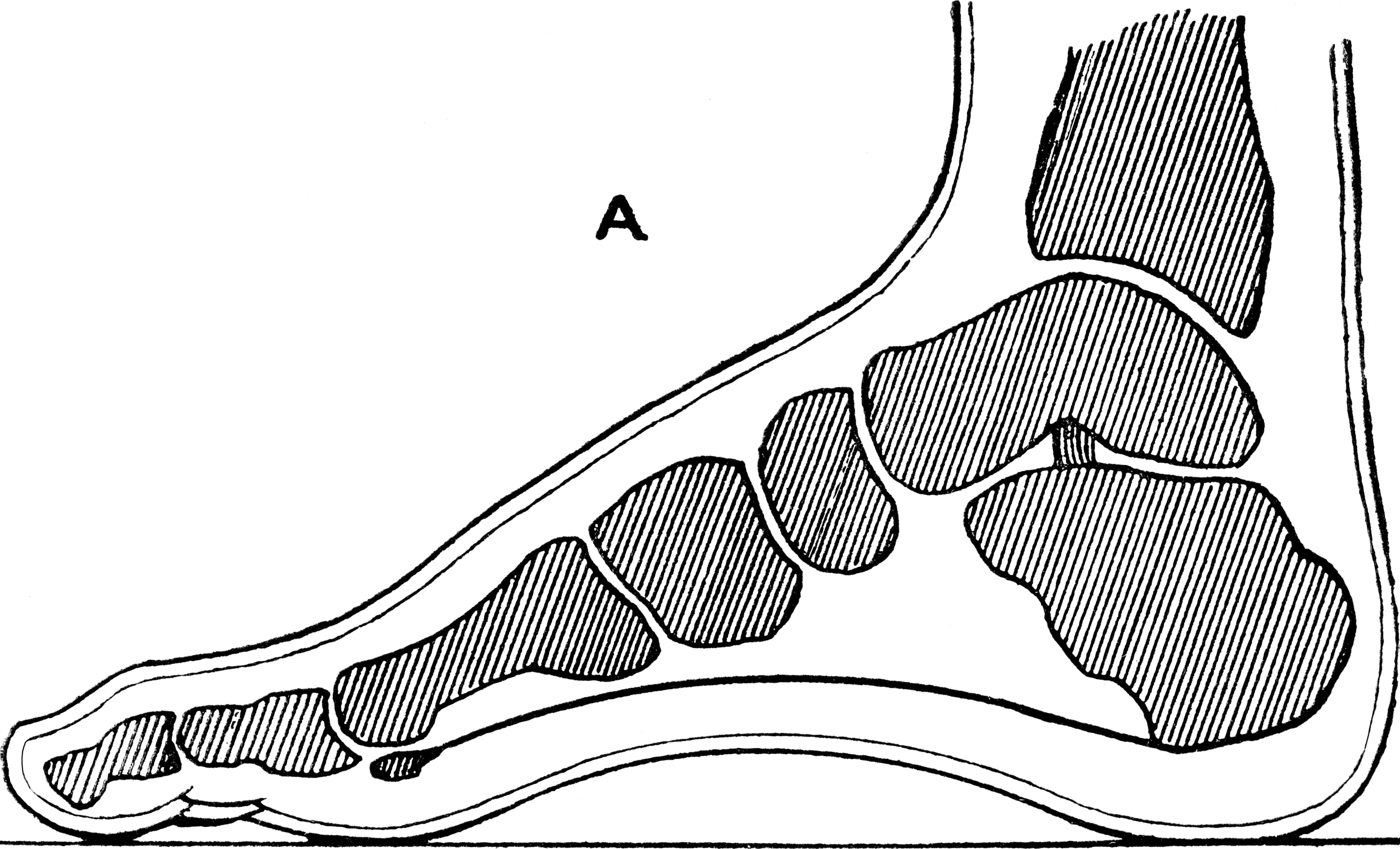
During the physical examination of a patient with calcaneal bursitis, the physician should keep the following considerations in mind. Swelling and redness of the posterior heel (the pump bump) may be clearly apparent. The inflamed area, which may be slightly warm to the touch, is generally tender to palpation. Careful examination can help the clinician to distinguish whether the inflammation is posterior to the Achilles tendon (within the subcutaneous calcaneal bursa) or anterior to the tendon (within the subtendinous calcaneal bursa). Differentiating Achilles tendinitis/tendinosis from bursitis may be impossible. At times, the 2 conditions co-exist. Isolated subtendinous calcaneal bursitis is characterized by tenderness that is best isolated by palpating just anterior to the medial and lateral edges of the distal Achilles tendon. Conversely, insertional Achilles tendinitis is notable for tenderness that is located slightly more distally, where the Achilles tendon inserts on the posterior calcaneus. A patient with plantar fasciitis has tenderness along the posterior aspect of the sole, but he/she should not have tenderness with palpation of the posterior heel or ankle. A patient with a complete avulsion or rupture of the Achilles tendon demonstrates a palpable defect in the tendon, weakness in plantarflexion, and a positive Thompson test on physical examination. During the Thompson test, the examiner squeezes the calf. The test is negative if this maneuver results in passive plantarflexion of the ankle, which would indicate that the Achilles tendon is at least partially intact.
Non Surgical Treatment
So what can you do to alleviate this type of pain in the foot? If the bursitis pain is occurring on the toes, bunion or back of the heel area the smart money would be on eliminating the shoes that seem to aggravate the condition. Eliminating these shoes may not in itself clear up the problem but you can be sure that if you continue to wear the offending shoes nothing you or your doctor do will permanently ?fix? the problem. A recurring theme that I use throughout this site that if you put an abnormally shaped foot in a dressy shoe it is literally the same as trying to put a square peg in a round hole, it will not fit. OK, so you threw away those dressy shoes and the foot still hurts, now what? Depending on the severity of the pain, over the counter anti-inflammatory medication may do the trick. The key here is to take the medication on an ongoing basis, according to the directions on the package to build up therapeutic blood levels. Assuming you can tolerate this type of medication, along with alternative treatments you can try). take the medication for 10-14 days. Stop if the symptoms have not dramatically improved. Icing the area during this period may also help reduce the symptoms.
Surgical Treatment
Surgery is rarely done strictly for treatment of a bursitis. If any underlying cause is the reason, this may be addressed surgically. During surgery for other conditions, a bursa may be seen and removed surgically.
Prevention
You can help to prevent heel pain and bursitis by maintaining a healthy weight, by warming up before participating in sports and by wearing shoes that support the arch of the foot and cushion the heel. If you are prone to plantar fasciitis, exercises that stretch the Achilles tendon (heel cord) and plantar fascia may help to prevent the area from being injured again. You also can massage the soles of your feet with ice after stressful athletic activities. Sometimes, the only interventions needed are a brief period of rest and new walking or running shoes.
Contracted Big Toe
 Overview
Overview
Hammer toe deformities can be painful and unsightly. These toe deformities can be the result of a muscle/tendon imbalance or often the end stage result of some systemic disease such as diabetes or arthritis, especially Rheumatoid arthritis. Hammertoe deformities are progressive and can be prevented.
Causes
The main cause of hammer toe is poorly fitted and/or poorly designed footwear. Any footwear that is too tight in the toe box, especially high-heeled shoes, can push the toes forward, crowding one or more of them into a space that is not large enough to allow hammertoes the toes to lie flat and spread as they should. Other causes include the following. Changes in foot anatomy. Sometimes the metatarsal bones in the ball of the foot can ?drop,? creating a situation in which the toes do not make contact with the surface of the shoe. The toes may then contract at one or both of the joints to re-establish contact with the surface. Traumatic injuries in which toes are jammed or broken. Diabetic neuropathy. This can cause abnormal foot biomechanics due to nerve and/or muscle damage. Damage to nerves and muscles from other conditions, such as arthritis or stroke. Heredity.
 Symptoms
Symptoms
The symptoms of hammertoe include a curling toe, pain or discomfort in the toes and ball of the foot or the front of the leg, especially when toes are stretched downward. Thickening of the skin above or below the affected toe with the formation of corns or calluses. Difficulty finding shoes that fit well. In its early stages, hammertoe is not obvious. Frequently, hammertoe does not cause any symptoms except for the claw-like toe shape.
Diagnosis
The exam may reveal a toe in which the near bone of the toe (proximal phalanx) is angled upward and the middle bone of the toe points in the opposite direction (plantar flexed). Toes may appear crooked or rotated. The involved joint may be painful when moved, or stiff. There may be areas of thickened skin (corns or calluses) on top of or between the toes, a callus may also be observed at the tip of the affected toe beneath the toenail. An attempt to passively correct the deformity will help elucidate the best treatment option as the examiner determines whether the toe is still flexible or not. It is advisable to assess palpable pulses, since their presence is associated with a good prognosis for healing after surgery. X-rays will demonstrate the contractures of the involved joints, as well as possible arthritic changes and bone enlargements (exostoses, spurs). X-rays of the involved foot are usually performed in a weight-bearing position.
Non Surgical Treatment
Apply a commercial, non-medicated hammer toe pad around the bony prominence of the hammer toe to decrease pressure on the area. Wear a shoe with a deep toe box. If the hammer toe becomes inflamed and painful, apply ice packs several times a day to reduce swelling. Avoid heels more than two inches tall. A loose-fitting pair of shoes can also help protect the foot while reducing pressure on the affected toe, making walking a little easier until a visit to your podiatrist can be arranged. While this treatment will make the hammer toe feel better, it is important to remember that it does not cure the condition. A trip to the podiatrist's office will be necessary to repair the toe to allow for normal foot function. Avoid wearing shoes that are too tight or narrow. Children should have their shoes properly fitted on a regular basis, as their feet can often outgrow their shoes rapidly.
Surgical Treatment
In more advanced cases of hammer toe, or when the accompanying pain cannot be relieved by conservative treatment, surgery may be required. Different types of surgical procedures are performed to correct hammer toe, depending on the location and extent of the problem. Surgical treatment is generally effective for both flexible and fixed (rigid) forms of hammer toe. Recurrence following surgery may develop in persons with flexible hammer toe, particularly if they resume wearing poorly-fitted shoes after the deformity is corrected.
How To Get Rid Of Bunions Naturally
Overview
 A bunion is a combination of an enlargement of the joint at the base and side of the big toe as well as the big toe being angled towards the rest of the toes (this angulation is known as Hallux Valgus). A bunion can lead to other foot deformities and problems such as a hammer toe of the second toe, corns and calluses as well as ingrown toenails. So if the pain isn't enough of a driving factor, the chance of developing these further complications should outline the importance and urgency of seeking treatment with a podiatrist.
A bunion is a combination of an enlargement of the joint at the base and side of the big toe as well as the big toe being angled towards the rest of the toes (this angulation is known as Hallux Valgus). A bunion can lead to other foot deformities and problems such as a hammer toe of the second toe, corns and calluses as well as ingrown toenails. So if the pain isn't enough of a driving factor, the chance of developing these further complications should outline the importance and urgency of seeking treatment with a podiatrist.
Causes
The main cause of bunions is excessive pressure being placed on the front of the foot, and is usually the result of wearing high-heeled shoes with pointed toes. A study by the American Orthopaedic Foot and Ankle Society found that 88 percent of women in the United States wear shoes that are too small and that 55 percent of them have bunions. Overall, bunions are nine times more common in women than men. In some cases, bunions are hereditary; they also may be caused by arthritis or polio.
Symptoms
Corns and calluses may occur on the soles of the feet, in between toes and on the bunion joint. Stiffness can occur at the big toe due to secondary arthritis, this is known as Hallux Rigidus. Other foot conditions can occur such as in growing toenails and in severe cases the bunion joint may have a fluid filled sack called a bursitis. This can be very painful and can become infected.
Diagnosis
Looking at the problem area on the foot is the best way to discover a bunion. If it has the shape characteristic of a bunion, this is the first hint of a problem. The doctor may also look at the shape of your leg, ankle, and foot while you are standing, and check the range of motion of your toe and joints by asking you to move your toes in different directions A closer examination with weight-bearing X-rays helps your doctor examine the actual bone structure at the joint and see how severe the problem is. A doctor may ask about the types of shoes you wear, sports or activities (e.g., ballet) you participate in, and whether or not you have had a recent injury. This information will help determine your treatment.
Non Surgical Treatment
Pain is the main reason that you seek treatment for bunion. Analgesics may help. Inflammation it best eased via ice therapy and techniques or exercises that deload the inflammed structures. Anti-inflammatory medications may help. Your physiotherapist will use an array of treatment tools to reduce your pain and inflammation. These include ice, electrotherapy, acupuncture, deloading taping techniques, soft tissue massage and orthotics to off-load the bunion. As your pain and inflammation settles, your physiotherapist will turn their attention to restoring your normal toe and foot joint range of motion and muscle length. Treatment may include joint mobilisation and alignment techniques, massage, muscle and joint stretches, taping, a bunion splint or orthotic. Your physiotherapist is an expert in the techniques that will work best for you. Your foot posture muscles are vital to correct the biomechanics that causing your bunion to deteriorate. Your physiotherapist will assess your foot posture muscles and prescribe the best exercises for you specific to your needs. During this stage of your rehabilitation is aimed at returning you to your desired activities. Everyone has different demands for their feet that will determine what specific treatment goals you need to achieve. For some it be simply to walk around the block. Others may wish to run a marathon or return to a labour-intensive activity. Your physiotherapist will tailor your rehabilitation to help you achieve your own functional goals. Bunions will deform further with no attention. Plus, the bunion pain associated does have a tendency to return. The main reason is biomechanical. In addition to your muscle control, your physiotherapist will assess your foot biomechanics and may recommend either a temporary off-the shelf orthotic or refer you to a podiatrist for custom made orthotics. You should avoid wearing high heel shoes and shoes with tight or angular toe boxes. Your physiotherapist will guide you. 
Surgical Treatment
In severe hallux valgus bunion cases, the first long bone (metatarsal) in the foot dramatically shifts away from the second metatarsal, resulting in looseness and a large deformity. In severe bunion corrections, a surgery known as the Lapidus procedure realigns the first metatarsal into its natural position. Using screws, the surgery holds the bone stable so it does not shift again and reduces the change of the bunion returning to basically none. Surgery may also involve removing the enlarged portion of the bunion region, cutting and realigning the bone, and correcting the position of the tendons and ligaments. By using a special plate with Lapidus procedures, University Foot and Ankle Institute patients are able to put weight on their foot after only 2-3 weeks, rather than the typical 6-8 weeks of no weight.
Do You Know The Chief Reasons Behind Overpronation
Overpronation still continues to be misused and misunderstood. For example, there was a study that got a lot of recent mileage in the mainstream media and the blogosphere that claimed to show that foot pronation was not associated with injury risk. It was intriguing following comments on the study in mainstream media and in social media, especially the parroting of the press release without any critical appraisal. The study actually eliminated the ?overpronators? that were probably at high risk from the study then found that ?overpronation? was not a risk factor. What is more intriguing was that there was another study from around the same time that found the exact opposite. Clearly, the data on ?overpronation? and risk for injury in runners is mixed, so we need to rely on the more formal systematic reviews and meta-analyses of all the data. The most recent one of those concluded that ?overpronation? is just a small risk factor for running injury risk, but it is still statistically significant.

Causes
Over-pronation has different causes. Obesity, pregnancy, age or repetitive pounding on a hard surface can weaken the arch leading to over-pronation. Over-pronation is also very common with athletes, especially runners and most of them nowadays use orthotics inside their shoes. Over-pronation affects millions of people and contributes to a range of common complaints including sore, aching feet, ball of foot pain, heel Pain, achilles tendonitis, bunions, shin pain, tired, aching legs, knee pain and lower back pain. The most effective treatment solution for over-pronation is wearing an orthotic shoe insert. Orthotics correct over-pronation, thereby providing natural, lasting pain relief from many common biomechanical complaints.
Symptoms
Because pronation is a twisting of the foot, all of the muscles and tendons which run from the leg and ankle into the foot will be twisted. In over-pronation, resulting laxity of the soft tissue structures of the foot and loosened joints cause the bones of the feet shift. When this occurs, the muscles which attach to these bones must also shift, or twist, in order to attach to these bones. The strongest and most important muscles that attach to our foot bones come from our lower leg. So, as these muscles course down the leg and across the ankle, they must twist to maintain their proper attachments in the foot. Injuries due to poor biomechanics and twisting of these muscles due to over-pronation include: shin splints, Achilles Tendonitis, generalized tendonitis, fatigue, muscle aches and pains, cramps, ankle sprains, and loss of muscular efficiency (reducing walking and running speed and endurance). Foot problems due to over-pronation include: bunions, heel spurs, plantar fasciitis, fallen and painful arches, hammer toes, and calluses.
Diagnosis
Look at your soles of your footwear: Your sneaker/shoes will display heavy wear marks on the outside portion of the heel and the inside portion above the arch up to the top of the big toe on the sole. The "wet-foot" test is another assessment. Dip the bottom of your foot in water and step on to a piece of paper (brown paper bag works well). Look at the shape of your foot. If you have a lot of trouble creating an arch, you likely overpronate. An evaluation from a professional could verify your foot type.
Non Surgical Treatment
Over-Pronation can be treated conservatively (non-surgical treatments) with over-the-counter orthotics. These orthotics should be designed with appropriate arch support and medial rearfoot posting to prevent the over-pronation. Footwear should also be examined to ensure there is a proper fit. Footwear with a firm heel counter is often recommended for extra support and stability. Improper fitting footwear can lead to additional problems of the foot. If the problem persists, call your doctor to schedule an appointment.
Prevention
With every step we take, we place at least half of our body weight on each foot (as we walk faster, or run, we can exert more than twice our body weight on each foot). As this amount of weight is applied to each foot there is a significant shock passed on to our body. Custom-made orthotics will absorb some of this shock, helping to protect our feet, ankles, knees, hips, and lower back.
The Best Way To Spot Calcaneal Apophysitis?
Sever's disease is a condition characterized by pain in one or both heels with walking. The pain is caused by shortening of the heel-cord. It usually affects children between the ages of 10 and 13 years old. During this phase of life, growth of the bone is taking place at a faster rate than the tendons. Sever's disease is also called calcaneal apophysitis.
Causes
Apart from age, other factors that may contribute to developing Sever?s disease include physical activity, any form of exercise that is weight bearing through the legs or stresses the soft tissue can exacerbate the pain of the disease, External factors, for example, running on hard surfaces or wearing inappropriate shoes during sport Overuse injury, very active children may repeatedly but subtly injure the bones, muscles and tendons of their feet and ankles. In time, the accumulated injuries cause symptoms.
Symptoms
The most prominent symptom of Sever's disease is heel pain which is usually aggravated by physical activity such as walking, running or jumping. The pain is localised to the posterior and plantar side of the heel over the calcaneal apophysis. Sometimes, the pain may be so severe that it may cause limping and interfere with physical performance in sports. External appearance of the heel is almost always normal, and signs of local disease such as edema, erythema (redness) are absent. The main diagnostic tool is pain on medial- lateral compression of the calcaneus in the area of growth plate, so called squeeze test. Foot radiographs are usually normal. Therefore the diagnosis of Sever's disease is primarily clinical.
Diagnosis
Sever condition is diagnosed by detecting the characteristic symptoms and signs above in the older children, particularly boys between 8 and 15 years of age. Sometimes X-ray testing can be helpful as it can occasionally demonstrate irregularity of the calcaneus bone at the point where the Achilles tendon attaches.
Non Surgical Treatment
Reduce activity, avoid going barefoot, and cushion the child's heel with shock absorbency. It is very important that your child wear shoes with padded heel surfaces and shoes with good arch supports even when not participating in sports. A heel cup or soft pediatric shoe insert is very important to reduce the pull from the calf muscles on the growth plate and to increase shock absorption and reduce irritation. The use of an ice pack after activity for 20 minutes is often useful. Your health care provider may also prescribe anti-inflammatory drugs or custom orthotics.
Surgical Treatment
The surgeon may select one or more of the following options to treat calcaneal apophysitis. Reduce activity. The child needs to reduce or stop any activity that causes pain. Support the heel. Temporary shoe inserts or custom orthotic devices may provide support for the heel. Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation. Physical therapy. Stretching or physical therapy modalities are sometimes used to promote healing of the inflamed issue. Immobilization. In some severe cases of pediatric heel pain, a cast may be used to promote healing while keeping the foot and ankle totally immobile. Often heel pain in children returns after it has been treated because the heel bone is still growing. Recurrence of heel pain may be a sign of calcaneal apophysitis, or it may indicate a different problem. If your child has a repeat bout of heel pain, be sure to make an appointment with your foot and ankle surgeon.
Achilles Tendon Rupture Clinical Tests For Diabetes
Overview
 When the Achilles tendon ruptures. it gets completely torn by a sudden movement of the ankle/leg. It usually occurs in a tendon that is worn out and has weakened over time and then suddenly tears when there is enough force. It typically occurs during recreational sports that involve running, jumping, and pivoting, such as basketball, soccer or racquet sports. It is most often seen in men in their 30s and 40s. Some medications and medical problems can predispose to having an Achilles rupture.
When the Achilles tendon ruptures. it gets completely torn by a sudden movement of the ankle/leg. It usually occurs in a tendon that is worn out and has weakened over time and then suddenly tears when there is enough force. It typically occurs during recreational sports that involve running, jumping, and pivoting, such as basketball, soccer or racquet sports. It is most often seen in men in their 30s and 40s. Some medications and medical problems can predispose to having an Achilles rupture.
Causes
Often an Achilles rupture can occur spontaneously without any prodromal symptoms. Unfortunately the first "pop" or "snap" that you experience is your Achilles tendon rupture. Achilles tendon rupture most commonly occurs in the middle-aged male athlete (the weekend warrior who is engaging in a pickup game of basketball, for example). Injury often occurs during recreational sports that require bursts of jumping, pivoting, and running. Most often these are tennis, racquetball, squash, basketball, soccer, softball and badminton. Achilles rupture can happen in the following situations. You make a forceful push-off with your foot while your knee is straightened by the powerful thigh muscles. One example might be starting a foot race or jumping. You suddenly trip or stumble, and your foot is thrust in front to break a fall, forcefully over stretching the tendon. You fall from a significant height. It does appear that previous history of Achilles tendonitis results in a degenerative tendon, which can grow weak and thin with age and lack of use. Then it becomes prone to injury or rupture. Certain illnesses (such as arthritis and diabetes) and medications (such as corticosteroids and some antibiotics) can also increase the risk of rupture.
Symptoms
Patients who suffer an acute rupture of the Achilles tendon often report hearing a "pop" or "snap." Patients usually have severe pain the back of the lower leg near the heel. This may or may not be accompanied by swelling. Additionally, because the function of the Achilles tendon is to enable plantarflexion (bending the foot downward), patients often have difficulty walking or standing up on their toes.
Diagnosis
The diagnosis of an Achilles tendon rupture is made entirely on physical examination. Often, there is a substantial defect in the Achilles from 2-5 cm before it inserts into the heel bone. However, the main test is to determine whether the Achilles has been ruptured is the Thompson test. This essentially involves placing the patient on their stomach and squeezing the calf muscle. If the Achilles is intact, the foot will rise [plantar flex]. If it is ruptured, the foot will not move and will tend to be in a lower lying position.
Non Surgical Treatment
Nonsurgical method is generally undertaken in individuals who are old, inactive, and at high-risk for surgery. Other individuals who should not undergo surgery are those who have a wound infection/ulcer around the heel area. A large group of patients who may not be candidates for surgery include those with diabetes, those with poor blood supply to the foot, patients with nerve problems in the foot, and those who may not comply with rehabilitation. Nonsurgical management involves application of a short leg cast to the affected leg, with the ankle in a slightly flexed position. Maintaining the ankle in this position helps appose the tendons and improves healing. The leg is placed in a cast for six to 10 weeks and no movement of the ankle is allowed. Walking is allowed on the cast after a period of four to six weeks. When the cast is removed, a small heel lift is inserted in the shoe to permit better support for the ankle for an additional two to four weeks. Following this, physical therapy is recommended. The advantages of a nonsurgical approach are no risk of a wound infection or breakdown of skin and no risk of nerve injury. The disadvantages of the nonsurgical approach includes a slightly higher risk of Achilles tendon rupture and the surgery is much more complex if indeed a repair is necessary in future. In addition, the recuperative period after the nonsurgical approach is more prolonged. 
Surgical Treatment
Surgery to repair an Achilles tendon rupture is performed under a spinal or general anaesthetic. During surgery the surgeon makes an incision in the skin over the ruptured portion of the tendon. The tendon ends are located and joined together with strong sutures (stitches), allowing the tendon to closely approximate its previous length. The skin is then closed with sutures and the foot is immobilised in a cast or splint, again in the toes-pointed position. Seven to ten days after surgery the cast or splint is removed in order for the sutures in the skin to be removed. Another cast or splint will be applied and will stay in place a further 5 - 7 weeks.
Prevention
There are things you can do to help prevent an Achilles tendon injury. You should try the following. Cut down on uphill running. Wear shoes with good support that fit well. Always increase the intensity of your physical activity slowly. Stop exercising if you feel pain or tightness in the back of your calf or heel.
Leg Length Discrepancy Women
The majority of people in the world actually have some degree of leg length discrepancy, up to 2cm. One study found that only around 1/4 of people have legs of equal lengths. LLD of greater than 2cm is relatively rare, however, and the greater the discrepancy, the greater the chances of having a clinical problem down the road. A limp generally begins when LLD exceeds 2cm and becomes extremely noticeable above 3cm. When patients with LLD develop an abnormal gait, one of the debilitating clinical features can be fatigue because of the relatively high amount of energy needed to walk in the new, inefficient way. Poliomyelitis, or polio, as it is more commonly known, used to account for around 1/3 of all cases of LLD, but due to the effectiveness of polio vaccines, it now represents a negligible cause of the condition. Functional LLD, described above, usually involves treatment focused on the hip, pelvis, and/or lower back, rather than the leg. If you have been diagnosed with functional LLD or pelvic obliquity, please ask your orthopaedic surgeon for more information about treatment of these conditions.

Causes
Sometimes the cause of LLD is unknown, yet the pattern or combination of conditions is consistent with a certain abnormality. Examples include underdevelopment of the inner or outer side of the leg (hemimelias) or (partial) inhibition of growth of one side of the body of unknown cause (hemihypertrophy). These conditions are present at birth, but the limb length difference may be too small to be detected. As the child grows, the LLD increases and becomes more noticeable. In hemimelia, one of the two bones between the knee and the ankle (tibia or fibula) is abnormally short. There also may be associated foot or knee abnormalities. Hemihypertrophy or hemiatrophy are rare conditions in which there is a difference in length of both the arm and leg on only one side of the body. There may also be a difference between the two sides of the face. Sometimes no cause can be found. This type of limb length is called idiopathic. While there is a cause, it cannot be determined using currect diagnostic methods.
Symptoms
Many people walk around with LLD?s of up to 2 cm. and not even know it. However, discrepancies above 2 cm. becomes more noticeable, and a slight limp is present. But even up to 3 cm. a small lift compensates very well, and many patients are quite happy with this arrangement. Beyond 3 cm. however, the limp is quite pronounced, and medical care is often sought at that point. Walking with a short leg gait is not only unsightly, but increases energy expenditure during ambulation. It could also put more stress on the long leg, and causes functional scoliosis. Where the discrepancy is more severe, walking becomes grotesque or virtually impossible.
Diagnosis
Leg length discrepancy may be diagnosed during infancy or later in childhood, depending on the cause. Conditions such as hemihypertrophy or hemiatrophy are often diagnosed following standard newborn or infant examinations by a pediatrician, or anatomical asymmetries may be noticed by a child's parents. For young children with hemihypertophy as the cause of their LLD, it is important that they receive an abdominal ultrasound of the kidneys to insure that Wilm's tumor, which can lead to hypertrophy in the leg on the same side, is not present. In older children, LLD is frequently first suspected due to the emergence of a progressive limp, warranting a referral to a pediatric orthopaedic surgeon. The standard workup for LLD is a thorough physical examination, including a series of measurements of the different portions of the lower extremities with the child in various positions, such as sitting and standing. The orthopaedic surgeon will observe the child while walking and performing other simple movements or tasks, such as stepping onto a block. In addition, a number of x-rays of the legs will be taken, so as to make a definitive diagnosis and to assist with identification of the possible etiology (cause) of LLD. Orthopaedic surgeons will compare x-rays of the two legs to the child's age, so as to assess his/her skeletal age and to obtain a baseline for the possibility of excessive growth rate as a cause. A growth chart, which compares leg length to skeletal age, is a simple but essential tool used over time to track the progress of the condition, both before and after treatment. Occasionally, a CT scan or MRI is required to further investigate suspected causes or to get more sophisticated radiological pictures of bone or soft tissue.
Non Surgical Treatment
People with uneven leg lengths may be more prone to pain in their back, hips, and knees; uneven gait; and lower leg and foot problems. Due to its risks, surgery is typically not recommended unless the difference is greater than one inch. In cases where the difference is less than one inch, providing the same support for both feet is the most effective. This can be achieved by getting custom-fitted orthotics for both feet. Orthotics are inserts that you wear in the shoes. Your chiropractor will request to measure your feet and possibly your legs. You can step on a device that will take the measurements or you might have a plaster cast of your feet taken. Orthotics are typically made from plastic and leather, and function biomechanically with your foot. If a leg length discrepancy is not properly corrected with orthotics, your chiropractor may recommend a heel lift, also known as a shoe lift. You simply place it in the back of your shoe along with the orthotic. Typically, you will only wear the heel lift in one shoe to assist the shorter leg.

Surgical Treatment
The bone is lengthened by surgically applying an external fixation device to the leg. The external fixator, a scaffold-like frame, is connected to the bone with wires, pins, or both. A small crack is made in the bone and the frame creates tension when the patient or family member turns its dial. This is done several times each day. The lengthening process begins approximately five to 10 days after surgery. The bone may lengthen 1 millimeter per day, or approximately 1 inch per month. Lengthening may be slower in a bone that was previously injured. It may also be slower if the leg was operated on before. Bones in patients with potential blood vessel abnormalities, such as cigarette smokers, may also need to be lengthened more slowly. The external fixator is worn until the bone is strong enough to support the patient safely. This usually takes about three months for each inch. Factors such as age, health, smoking and participation in rehabilitation can affect the amount of time needed.